The infant’s gut microbiota begins to develop at birth, via contact with the mother’s vaginal and intestinal microbiota, through skin contact and during breast-feeding. 1Wopereis H, Oozeer R, Knipping K, Belzer C, Knol J. The first thousand days – intestinal microbiology of early life: establishing a symbiosis. Pediatr Allergy Immunol. Published on … Continue reading,2Scholtens P, Oozeer R, Martin R, Amor K, Knol J. The early settlers: intestinal microbiology in early life. Annu Rev Food Sci Technol. Published on 2012;3:425-447
After birth, the infant’s skin, oral cavity and respiratory tract come into direct contact with the external world, leading to continuous exposure to microorganisms.3Wopereis H, Oozeer R, Knipping K, Belzer C, Knol J. The first thousand days – intestinal microbiology of early life: establishing a symbiosis. Pediatr Allergy Immunol. Published on … Continue reading This increase in environmental exposure means the infant must rapidly develop a healthy and resilient immune system.4Simon A, Hollander G, McMichael A, Evolution of the immune system in humans from infancy to old age. Proc Biol Sci. Published on 2015;282(1821):20143085
Human milk is best for infants
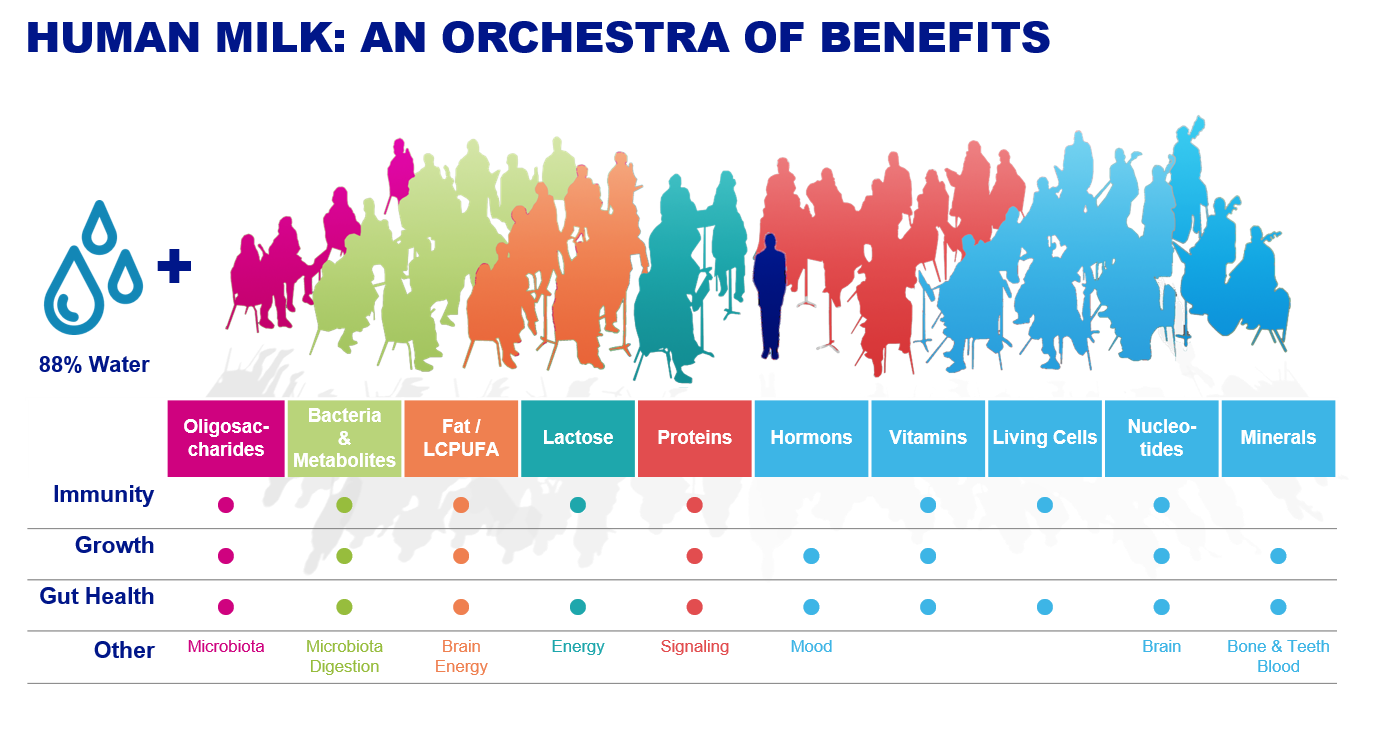
Human milk is the best source of nutrition for infants, as it provides a complex and diverse matrix of nutritional and bioactive compounds in an optimal balance of nutrients and other components that are specifically tailored to the infant’s needs.5WHO Growth Standards. Published on 2006 http://www.who.int/childgrowth/en/.
Human milk is one of the first and most important factors in establishing the infant’s immune system. It acts as an “inoculum” for the infant’s gut, priming the immune cells to respond appropriately to food, antigens, pathogens, and commensal bacteria.6Jeurink P, van B, Jiménez E, et al. Human milk: a source of more life than we imagine. Benef Microbes. Published on 2013;4(1):17-30.
Human milk helps establish a healthy gut and immune system
The beneficial effects of human milk are due to its many bioactive compounds. These include:7Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am. Published on 2013;60:49-74
- Human milk oligosaccharides (HMOS)
- Bacteria and their metabolites (such as bifidobacteria and lactobacilli)
- Vitamins
- Minerals
- Immune cells
Of the many compounds of human milk, oligosaccharides, bacteria and bioactive compounds produced by bacteria play a key role in the development of a healthy gut microbiota and immune system.
Oligosaccharides in human milk have a “prebiotic” effect
Human milk contains a relatively large number of oligosaccharides (Human Milk Oligosaccharides, HMOS).8Thurl S, Munzert M, Boehm G, Matthews C, Stahl B. Systematic review of the concentrations of oligosaccharides in human milk. Nutr Rev. Published on 2017;75(11):920-933 HMOS represent the third largest component of milk solids after lactose and lipids.9Jantscher-Krenn E, Bode L. Human milk oligosaccharides and their potential benefits for the breast-fed neonate. Minerva Pediatr. Published on 2012;64(1):83-99
More than 200 different oligosaccharides have been identified in human milk and they have an overall “prebiotic” effect. This means that they pass undigested into the lower part of the gastrointestinal tract where they promote the growth of beneficial microorganisms, such as bifidobacteria and lactobacilli.10Boehm G, Stahl B. Oligosaccharides from milk. J Nutr Published on 2007;137:847S-849S The International Scientific Association for Probiotics and Prebiotics (ISAPP) has published the definition for prebiotics in a consensus statement in June 2017, stating “a prebiotic is a substrate that is selectively utilized by host microorganisms conferring a health benefit”.
The total pool of HMOS as a collective group supports immune health, as they prevent pathogen to cause infection, and increase the number and activity of immune cells to fight against.11Ayechu-Muruzabal V, van S, Mank M, et al. Diversity of Human Milk Oligosaccharides and Effects on Early Life Immune Development. Front Pediatr. Published on 2018;6:239
Bacteria in human milk and their metabolites
Human milk contains viable and non-viable bacterial cells and fragments, e.g. Streptococcus, Staphylococcus, Lactobacillus and Bifidobacterium.12Jost T, Lacroix C, Braegger C, Chassard C. Assessment of bacterial diversity in breast milk using culture-dependent and culture-independent approaches. Br J Nutr. Published on 2013;110(7):1253-1262 ,13Bergmann H, Rodríguez J, Salminen S, Szajewska H. Probiotics in human milk and probiotic supplementation in infant nutrition: a workshop report. Br J Nutr. Published on 2014;112(7):1119-1128 ,14Hunt K, Foster J, Forney L, et al. Characterization of the diversity and temporal stability of bacterial communities in human milk. PLoS One. Published on 2011;6(6):e21313
There is a high variability in composition and number of bacteria per millilitre human milk among mothers and in some cases even within mothers at different time points.15Boix-Amorós A, Collado M, Mira A. Relationship between Milk Microbiota, Bacterial Load, Macronutrients, and Human Cells during Lactation. Front Microbiol. Published on 2016;7:492 Moreover, the total number of bacteria in human milk significantly differs according to detection methods. It has been estimated that human milk contains between 103 and 106 bacteria per millilitre.16Boix-Amorós A, Collado M, Mira A. Relationship between Milk Microbiota, Bacterial Load, Macronutrients, and Human Cells during Lactation. Front Microbiol. Published on 2016;7:492 ,17Heikkilä M, Saris P. Inhibition of Staphylococcus aureus by the commensal bacteria of human milk. J Appl Microbiol. Published on 2003;95(3):471-478 The difference in number due to different detection methods, could be due to the fact that in molecular based methods, also DNA form non-viable bacteria and extracellular DNA can be amplified, suggesting not only live bacteria but significant amounts of non-viable bacteria in human milk.18Boix-Amorós A, Collado M, Mira A. Relationship between Milk Microbiota, Bacterial Load, Macronutrients, and Human Cells during Lactation. Front Microbiol. Published on 2016;7:492
Although the composition and numbers of bacteria vary widely among individuals, human milk is now considered to be an important source of beneficial “probiotic” bacteria in the crucial first days and weeks of an infant’s life. The milk microbiome may thus be regarded as an inoculum for the infant’s gut, being essential in programming the immune system to respond appropriately to (food-)antigens, pathogens and commensal bacteria.19(Donnet-Hughes et al. 2010, Perez-Cano et al. 2010, Maldonado et al. Published on 2012, Martin et al. 2010)
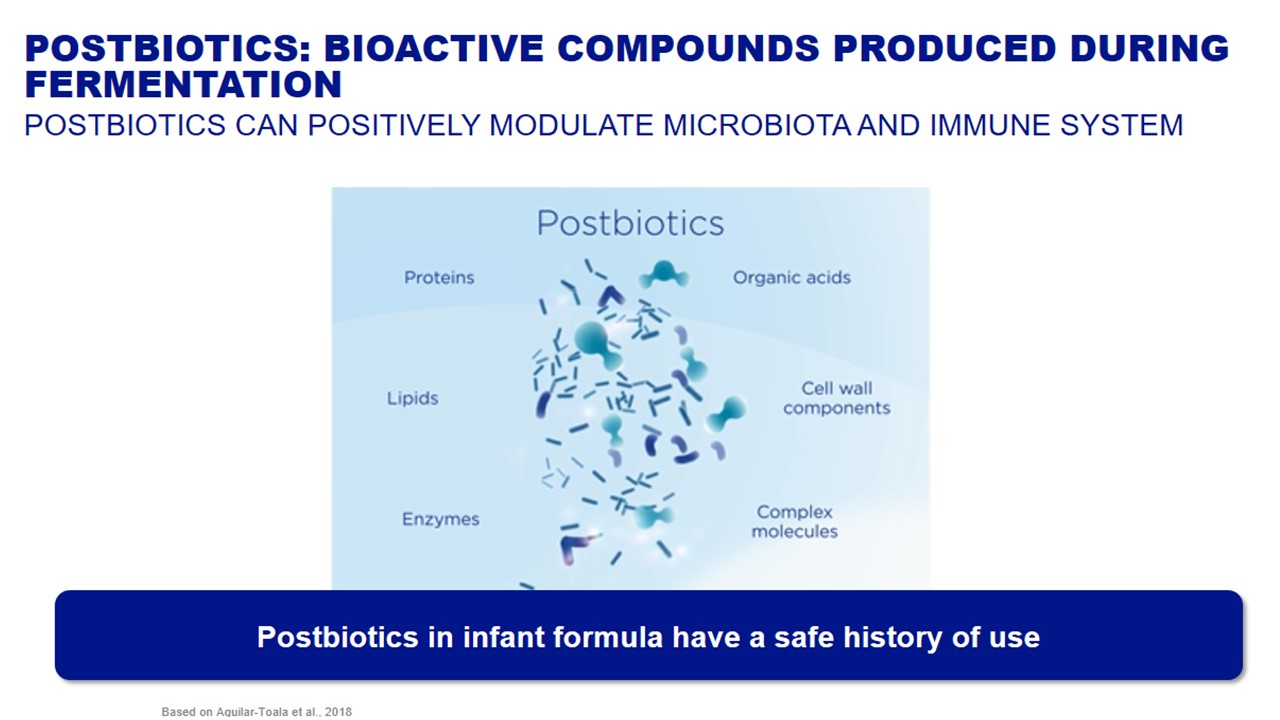
Interestingly, the immunomodulatory activities of bacteria are also associated to the bioactive compounds produced by these bacteria. Postbiotics refer to these products or by-products secreted by bacteria. During fermentation bacteria metabolize food and produce various bacterial compounds and metabolites20Aguilar-Toalá JE, Garcia-Varela R, Garcia HS, et al. Postbiotics: An evolving term within the functional foods field. T. Published on 2018;75:105-114. doi :10.1016/j.tifs.2018.03.009. Each bacterial strain used during specific fermentation processes produce unique postbiotics and therefore postbiotics from other bacterial strains or produced with another fermentation process cannot be compared.
The various compounds produced as postbiotics are included in the Figure below:
Although the importance of postbiotics has relatively been overlooked, scientific evidence of their beneficial health effects is progressively increasing.
View References
| 1, 3 | Wopereis H, Oozeer R, Knipping K, Belzer C, Knol J. The first thousand days – intestinal microbiology of early life: establishing a symbiosis. Pediatr Allergy Immunol. Published on 2014;25(5):428-438 |
|---|---|
| 2 | Scholtens P, Oozeer R, Martin R, Amor K, Knol J. The early settlers: intestinal microbiology in early life. Annu Rev Food Sci Technol. Published on 2012;3:425-447 |
| 4 | Simon A, Hollander G, McMichael A, Evolution of the immune system in humans from infancy to old age. Proc Biol Sci. Published on 2015;282(1821):20143085 |
| 5 | WHO Growth Standards. Published on 2006 http://www.who.int/childgrowth/en/. |
| 6 | Jeurink P, van B, Jiménez E, et al. Human milk: a source of more life than we imagine. Benef Microbes. Published on 2013;4(1):17-30. |
| 7 | Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am. Published on 2013;60:49-74 |
| 8 | Thurl S, Munzert M, Boehm G, Matthews C, Stahl B. Systematic review of the concentrations of oligosaccharides in human milk. Nutr Rev. Published on 2017;75(11):920-933 |
| 9 | Jantscher-Krenn E, Bode L. Human milk oligosaccharides and their potential benefits for the breast-fed neonate. Minerva Pediatr. Published on 2012;64(1):83-99 |
| 10 | Boehm G, Stahl B. Oligosaccharides from milk. J Nutr Published on 2007;137:847S-849S |
| 11 | Ayechu-Muruzabal V, van S, Mank M, et al. Diversity of Human Milk Oligosaccharides and Effects on Early Life Immune Development. Front Pediatr. Published on 2018;6:239 |
| 12 | Jost T, Lacroix C, Braegger C, Chassard C. Assessment of bacterial diversity in breast milk using culture-dependent and culture-independent approaches. Br J Nutr. Published on 2013;110(7):1253-1262 |
| 13 | Bergmann H, Rodríguez J, Salminen S, Szajewska H. Probiotics in human milk and probiotic supplementation in infant nutrition: a workshop report. Br J Nutr. Published on 2014;112(7):1119-1128 |
| 14 | Hunt K, Foster J, Forney L, et al. Characterization of the diversity and temporal stability of bacterial communities in human milk. PLoS One. Published on 2011;6(6):e21313 |
| 15, 16, 18 | Boix-Amorós A, Collado M, Mira A. Relationship between Milk Microbiota, Bacterial Load, Macronutrients, and Human Cells during Lactation. Front Microbiol. Published on 2016;7:492 |
| 17 | Heikkilä M, Saris P. Inhibition of Staphylococcus aureus by the commensal bacteria of human milk. J Appl Microbiol. Published on 2003;95(3):471-478 |
| 19 | (Donnet-Hughes et al. 2010, Perez-Cano et al. 2010, Maldonado et al. Published on 2012, Martin et al. 2010) |
| 20 | Aguilar-Toalá JE, Garcia-Varela R, Garcia HS, et al. Postbiotics: An evolving term within the functional foods field. T. Published on 2018;75:105-114. doi :10.1016/j.tifs.2018.03.009 |