Infants and young children have very different nutritional needs compared with adults;1Gluckman PD, Hanson MA. Semin Fetal Neonatal Med. Published on 2004;9(5):419-25 preterm infants are in need of even greater nutritional support because of suboptimal foetal development.2Klein. J Nutr. Published on 2002;132:1395S-577S.
Find out more about our research in preterm nutrition here.
Nutrition during early life has key impact on physical growth, cognitive development, immune maturation, development of digestive systems, and development of healthy eating habits of the infant.3Unicef, The state of the World’s Children. Published on 2001
At Danone Research & Innovation, we have a heritage of expertise and knowledge in the areas of growth and metabolism. Our passion is discovering more about how nutrition impacts growth, development and body composition in preterm and term infants, toddlers and mothers-to-be. We use these insights to develop nutritional products that enable optimal growth within these patient/consumer groups.

Through increasing our knowledge on the metabolic load (the effort required by the body to use or store nutrients), bioavailability, and kinetics of micro- and macronutrients, we have gained insight into the role of nutrition in the growth and development of term and preterm infants. In addition, we are unravelling the mechanisms underlying metabolic programming, e.g. sustained effects of early nutrition on later life metabolic health.
Early life nutrition influences quality of growth.
Emerging evidence exists that not only the total amount of body fat, but also the distribution of body fat, especially the deposition of visceral fat, determines the risk for metabolic and cardiovascular diseases in later life. Over the last few years, in close collaboration with international experts, we have explored the development of body composition and body fat distribution in early life using state-of-the-art, new developed measurement techniques.4Holzhauer S, et al. Eur J Epidemiol. Published on 2009;24(9):521-9 ,5Breij LM, et al. Pediatr Obes. Published on 2017;12(4):286-294 We observed that growth trajectories during the foetal and infancy period influence body fat distribution6Durmus B, et al. Clin Endocrinol (Oxf). Published on 2010;72(5):633-40 with lasting effects in childhood.7Vogelezang S, et al. Int J Obes (Lond). Published on 2016;40(4):595-600
These insights once more emphasise the importance of early life nutrition supporting this ‘quality of growth’ during the first 1000 days.
Research over the past decades has led to significant improvements in fat quality of infant formulas (e.g. by the addition of LC-PUFAs) as well as protein quality (casein-whey ratio) facilitating a reduction in total protein to better meet the nutritional needs of the growing (healthy) infant.
Nuturis® – our unique infant formula concept
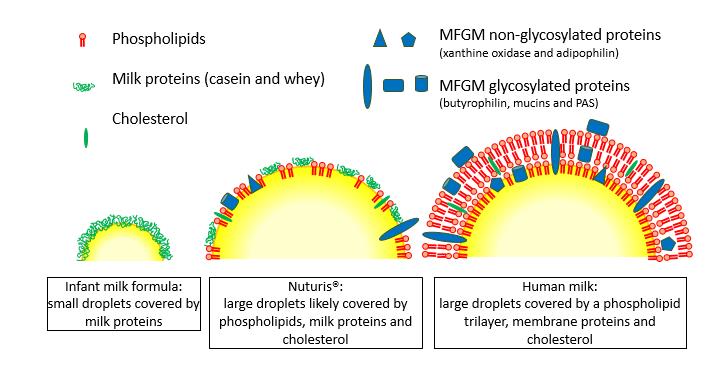
Dietary lipid structure influences the way lipids are absorbed and used in an infant’s body for energy use and storage.8Baumgartner, Eur J Clin Nutr. 2017. Apr 19. doi: Published on 10.1038/ejcn.2017.50. ,9Vors AM, J Clin Nutr. Published on . Published on 2013;97:23-6 /,10Michalski, EUR J LIPID SCI TECH. Published on 2009;111:413-31 This could partially explain the difference in growth and body composition development between formula-fed and human milk fed infants and the subsequent differences in risk for metabolic health complications or disorders in later life.11Dewey KG, et al. Am J Clin Nutr. Published on 1993:57;140-5 ,12Bergmann KE. et al. Int J Obes. Published on 2003;27:162-72 ,13Rzehak P, et al. Eur J Epidemiol. Published on 2009;24:449–467 /
Influencing body composition
At Danone Research & Innovation, we have developed a processing technique and added milk fat globule membrane to a concept formula. This has resulted in the patented nutritional innovation Nuturis®, large, phospholipid coated lipid droplets (mode diameter 3-5 μm) that mimic the structure of lipids in human milk.14Gallier, et al. Biointerfaces. Published on 2015;136:329–339 We have shown that infants fed Nuturis® displayed growth and body composition development more closely resembling that of breastfed infants.
View References
| 1 | Gluckman PD, Hanson MA. Semin Fetal Neonatal Med. Published on 2004;9(5):419-25 |
|---|---|
| 2 | Klein. J Nutr. Published on 2002;132:1395S-577S. |
| 3 | Unicef, The state of the World’s Children. Published on 2001 |
| 4 | Holzhauer S, et al. Eur J Epidemiol. Published on 2009;24(9):521-9 |
| 5 | Breij LM, et al. Pediatr Obes. Published on 2017;12(4):286-294 |
| 6 | Durmus B, et al. Clin Endocrinol (Oxf). Published on 2010;72(5):633-40 |
| 7 | Vogelezang S, et al. Int J Obes (Lond). Published on 2016;40(4):595-600 |
| 8 | Baumgartner, Eur J Clin Nutr. 2017. Apr 19. doi: Published on 10.1038/ejcn.2017.50. |
| 9 | Vors AM, J Clin Nutr. Published on . Published on 2013;97:23-6 / |
| 10 | Michalski, EUR J LIPID SCI TECH. Published on 2009;111:413-31 |
| 11 | Dewey KG, et al. Am J Clin Nutr. Published on 1993:57;140-5 |
| 12 | Bergmann KE. et al. Int J Obes. Published on 2003;27:162-72 |
| 13 | Rzehak P, et al. Eur J Epidemiol. Published on 2009;24:449–467 / |
| 14 | Gallier, et al. Biointerfaces. Published on 2015;136:329–339 |


