Nutritional ingredients such as specific pre- and probiotics can influence the immune system directly1Lehmann S, et al. PloS one. Published on 2015. 10(7):p. e0132304 and indirectly via modulation of the gut microbiota. 2Lehmann S, et al. PloS one. Published on 2015. 10(7):p. e0132304 ,3Druart, C et al. Advances in Nutrition: An International Review Journal. Published on 2014. 5(5): 624S-633S ,4Wopereis, H, et al. Pediatric Allergy and Immunology. Published on 2014. 25(5): 428-438 ,5Rachid, R. and T.A, Chatila. Current Opinion in Pediatrics. Published on 2016. 28(6): 748-753 ,6Muir, A.B, et al. Allergy. Published on 2016. 71(9):1256-1263 When given in early life, they can help create the optimal conditions for the immune system to be trained in the right way.
PREBIOTICS – scGOS/lcFOS (9:1)
Prebiotics are non-digestible dietary carbohydrates that travel to the colon intact and are able to selectively stimulate the growth and activity of beneficial bacteria.7Shamir R, et al. Essential Knowledge Briefing, Wiley, Chichester. Published on 2015
Prebiotic oligosaccharides are an abundant bioactive component in human milk. For infants who are unable to breastfeed, Danone Research & Innovation has developed a unique and patented blend of prebiotic – short-chain galacto-oligosaccharides and long chain fructo-oligosaccharides, namely scGOS/lcFOS (9:1). The health benefits of scGOS/lcFOS (9:1) in early life are validated in over 40 clinical studies, described in more than 75 scientific publications and include:
• Reduced incidence of allergic symptoms, such as atopic dermatitis8Arslanoglu, S, et al. J Nutr. Published on 2008. 138(6): p. 1091-5 ,9Arslanoglu, S del. et al. J Biol Regul Homeost Agents. Published on 2012. 26(3 Suppl): p. 49-59 ,10Moro, G et al. Arch Dis Child. Published on 2006. 91(10): p. 814-9
• Increased level of healthy gut bacteria and reduced level of potentially harmful bacteria11Haarman, M. and J. Knol, Appl Environ Microbiol. del. Published on 2005. 71(5): p. 2318-24
• Reduced occurrence of infections12Martin, R del. et al. Benef Microbes. Published on 2010. 1(4): p. 367 ,13Jeurink, P.V, et al. Benef Microbes. Published on 2013. 4(1): p. 17-30.]
• Improved stool frequency and consistency
We have also demonstrated the favourable health benefit of the use of this specific mixture of prebiotics results in positive short and long-term health economic benefits.14Lenoir-Wijnkoop et al. Eu J Health Econ. Published on 2012. 13:101-110

PREBIOTICS – scFOS-lcFOS (9:1)
Infants with severe Cow’s Milk Allergy (CMA) and Multiple Food Allergy (MFA) cannot tolerate even traces of cow’s milk. For those are unable to breastfeed, an infant formula containing an adapted prebiotic is required and oligofructose (scFOS) has been identified as a suitable alternative to scGOS:
• it is plant-derived;
• it is cow’s milk free;
• it promotes bifidobacteria and has a similar oligosaccharide structure to scGOS.

PROBIOTICS
Probiotics are live microrganisms, which when administered in adequate amounts, confer a health benefit on the host.15Shamir R, et al. Essential Knowledge Briefing, Wiley, Chichester. Published on 2015 As well as being found in common foodstuffs such as fermented milk, fermented vegetables and yoghurt, they are also present in human milk. In fact, human milk contains around 103-104 cfu/ml, making it rich source of potential commensal bacteria for the infant16Martín, R et al. The Journal of Pediatrics. Published on 2003. 143: 754-758 ,17Perez, P.F, et al. Pediatrics. Published on 2007. 119: e724-732
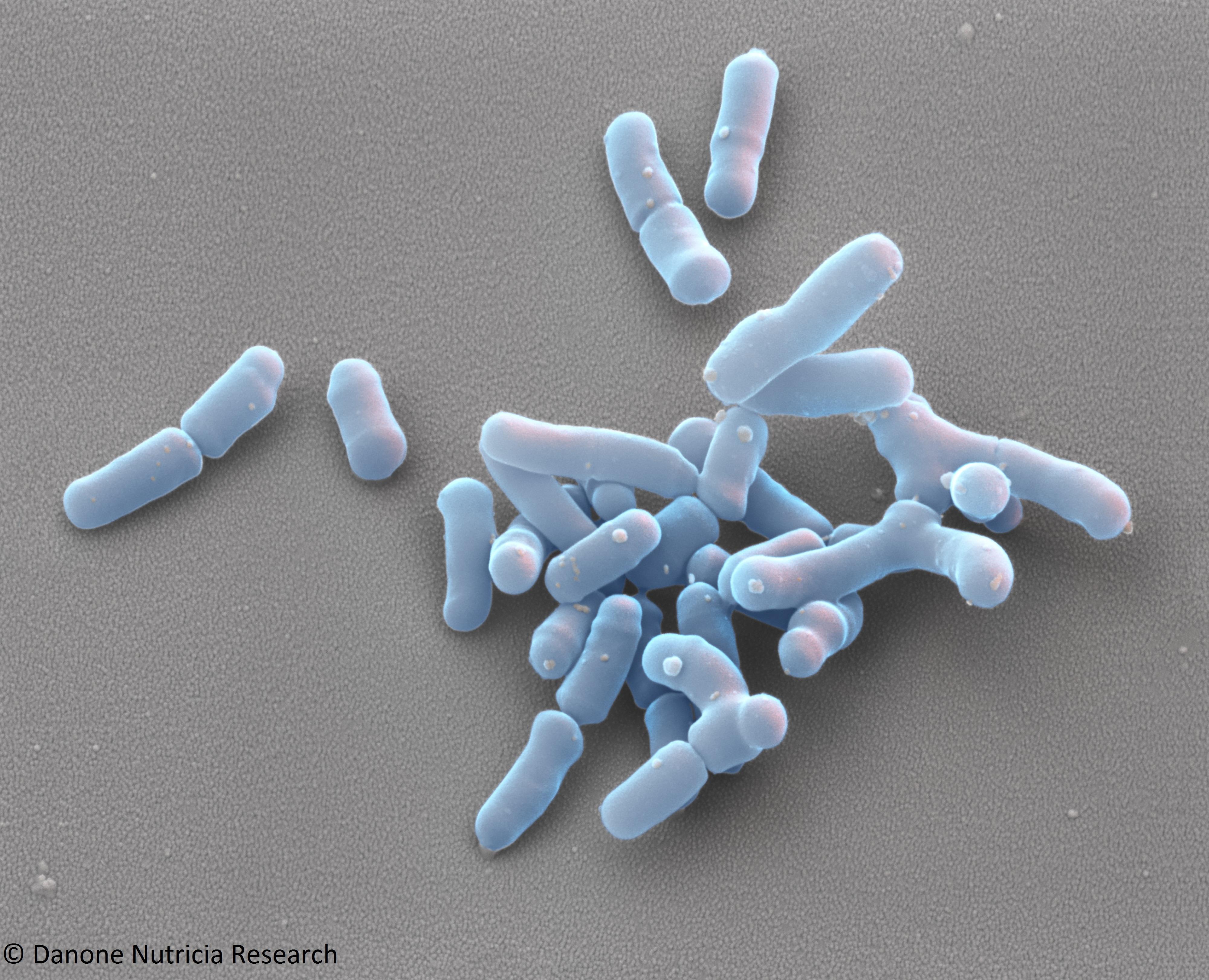
Bifidobacterium breve is commonly found in the gut of healthy breastfed infants and also in human milk. Our preclinical research has demonstrated that Bifidobacterium breve M-16V is the most promising strain in reducing allergic symptoms, and has been shown to have anti-allergic properties.18Hougee S, et al. Int Arch Allergy Immunol. Published on 2010. 151:107-117 It has also demonstrated synergistic benefits when combined with our unique prebiotic mixture scGOS/lcFOS (9:1).19van Esch BCAM, et al. Immunity, Inflammation and Disease. Published on 2016. 4(2): 155–165 ,20Schouten B, et al. J Nutr. Published on 2009. 139(7):1398-403 /
Selected among 400 different strains and supported by >17 clinical studies including preterms, since 1994, B Breve M16V has been clinically proven to:
• Improve allergic symptoms in infants with IgE-mediated atopic dermatitis21van der Aa, L.B, et al. Clin Exp Allergy. Published on 2010. 40(5): p. 795-804
• Improve diaper dermatitis and gastrointestinal symptoms22van der Aa, L.B, et al. Clin Exp Allergy. Published on 2010. 40(5): p. 795-804
• Prevent asthma-like symptoms23van der Aa, L.B et al. Allergy. Published on 2011. 66(2): p. 170-7
Read more about Our allergy research innovations
SYNBIOTICS: scGOS/lcFOS (9:1) or FOS/FOS + B breve M-16V
Synbiotics are a combination of pre and probiotics that work synergistically. At Danone Research & Innovation, we have developed a specific, synbiotic combination that acts synergistically, not only to resolve allergy symptoms in infants24Harvey, B.M et al. Pediatr Res. Published on 2014. 75(2): p. 343-51 ,25Burks, A.W del. et al. Pediatr Allergy Immunol. Published on 2015. 26(4): p. 316-22 /,26Michaelis, L. W, et al. Allergy, EAACI 2016 abstract book. Published on 2016. 71(S102): p. 3-94 but also to restore the composition of the gut microbiota to reflect that of healthy breastfed infants.27Michaelis, L. W, et al. Allergy, EAACI 2016 abstract book. Published on 2016. 71(S102): p. 3-94 ,28Haahtela T, et al. World Allergy Organization Journal. Published on 2013;6(1):3
Recent data has shown that it is safe and suitable for the use in the dietary management of CMA and that, after eight weeks of use, it results in a significantly higher percentage of faecal bifidobacteria compared to standard amino acid formula, without synbiotics. In addition, faecal bifidobacteria levels in infants using an amino acid formula with synbiotics are closer to levels seen in age-matched healthy subjects.29Candy, et al. Clin Trans Allergy. Published on 2017;7(1):10
View References
| 1, 2 | Lehmann S, et al. PloS one. Published on 2015. 10(7):p. e0132304 |
|---|---|
| 3 | Druart, C et al. Advances in Nutrition: An International Review Journal. Published on 2014. 5(5): 624S-633S |
| 4 | Wopereis, H, et al. Pediatric Allergy and Immunology. Published on 2014. 25(5): 428-438 |
| 5 | Rachid, R. and T.A, Chatila. Current Opinion in Pediatrics. Published on 2016. 28(6): 748-753 |
| 6 | Muir, A.B, et al. Allergy. Published on 2016. 71(9):1256-1263 |
| 7, 15 | Shamir R, et al. Essential Knowledge Briefing, Wiley, Chichester. Published on 2015 |
| 8 | Arslanoglu, S, et al. J Nutr. Published on 2008. 138(6): p. 1091-5 |
| 9 | Arslanoglu, S del. et al. J Biol Regul Homeost Agents. Published on 2012. 26(3 Suppl): p. 49-59 |
| 10 | Moro, G et al. Arch Dis Child. Published on 2006. 91(10): p. 814-9 |
| 11 | Haarman, M. and J. Knol, Appl Environ Microbiol. del. Published on 2005. 71(5): p. 2318-24 |
| 12 | Martin, R del. et al. Benef Microbes. Published on 2010. 1(4): p. 367 |
| 13 | Jeurink, P.V, et al. Benef Microbes. Published on 2013. 4(1): p. 17-30.] |
| 14 | Lenoir-Wijnkoop et al. Eu J Health Econ. Published on 2012. 13:101-110 |
| 16 | Martín, R et al. The Journal of Pediatrics. Published on 2003. 143: 754-758 |
| 17 | Perez, P.F, et al. Pediatrics. Published on 2007. 119: e724-732 |
| 18 | Hougee S, et al. Int Arch Allergy Immunol. Published on 2010. 151:107-117 |
| 19 | van Esch BCAM, et al. Immunity, Inflammation and Disease. Published on 2016. 4(2): 155–165 |
| 20 | Schouten B, et al. J Nutr. Published on 2009. 139(7):1398-403 / |
| 21, 22 | van der Aa, L.B, et al. Clin Exp Allergy. Published on 2010. 40(5): p. 795-804 |
| 23 | van der Aa, L.B et al. Allergy. Published on 2011. 66(2): p. 170-7 |
| 24 | Harvey, B.M et al. Pediatr Res. Published on 2014. 75(2): p. 343-51 |
| 25 | Burks, A.W del. et al. Pediatr Allergy Immunol. Published on 2015. 26(4): p. 316-22 / |
| 26, 27 | Michaelis, L. W, et al. Allergy, EAACI 2016 abstract book. Published on 2016. 71(S102): p. 3-94 |
| 28 | Haahtela T, et al. World Allergy Organization Journal. Published on 2013;6(1):3 |
| 29 | Candy, et al. Clin Trans Allergy. Published on 2017;7(1):10 |

