Allergy is an ‘immunological hypersensitivity’, and as such is referred to as an ‘immune-mediated’ disease. Allergic diseases in infancy and childhood are an early signal that the immune system has created an inadequate response and therefore can be considered imbalanced.1Prescott, S.L, Origins: Early-life solutions to the modern health crisis, Published on 2015: University of Western Australia Press, Crawly, Western Australia. This could provide an indication of an increased risk of developing other non-communicable diseases later in life, such as diabetes and chronic respiratory diseases.2Prescott SL, J Allergy Clin Immunol. Published on 2013;131(1):23-30 ,3Pawankar R, et al. World Allergy Organisation (WAO): White book on allergy. Wisconsin: World Allergy Organisation. Published on 2011 ,4Fiocchi A, et al. World Allergy Organization Journal. Published on 2010;3(4):57-161 ,5Gupta R, JAMA Pediatrics. Published on 2013;167:1026-31 ,6Patel DA J Allergy Clin Immunol. Published on 2011;128:110-5 ,7Sladkevicius E and Guest JF, J Med Econom. Published on 2010;13:273-83 ,8Boyle Allergy, Published on 2016;71:701-710
Allergies occur when the immune system overreacts to substances that are usually harmless, such as foods, pollen, or pet dander. Early life, from pregnancy, through to infancy and childhood, presents an important window of opportunity to positively modify the developing immune system. A well developed immune system is of key importance to ensure the maintenance of health for infants and children, throughout life.9Prescott SL, J Allergy Clin Immunol. Published on 2013;131(1):23-30 
Modern life challenges the developing immune system
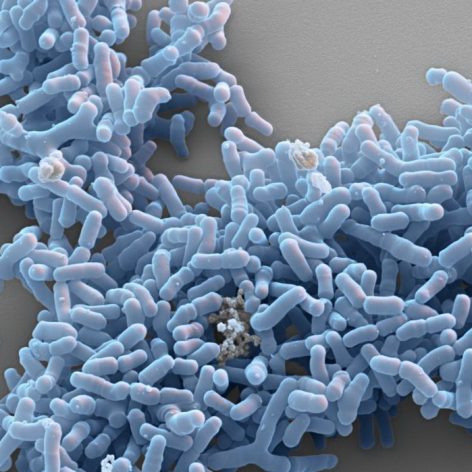
The incidence of allergy is on the rise, with up to 40% of the world’s population now affected.10Prescott SL, J Allergy Clin Immunol. Published on 2013;131(1):23-30 ,11Pawankar R, et al. World Allergy Organisation (WAO): White book on allergy. Wisconsin: World Allergy Organisation. Published on 2011 It is thought the rising allergy epidemic is due to the vulnerability of the developing immune system to meet the challenges related to modern life.12Prescott SL, J Allergy Clin Immunol. Published on 2013;131(1):23-30 Although our immune systems have evolved to deal with changes in our environment, the world may be changing faster than our immune systems can adapt. These modern changes include pollution, the widespread use of antibiotics and increasing number of caeserian-section deliveries. Each of these changes can trigger an imbalance – or ‘dysbiosis’ – of the gut microbiota.13Prescott SL, J Allergy Clin Immunol. Published on 2013;131(1):23-30 ,14Kim BJ et al. Environmental changes, microbiota and allergic diseases. Allergy, Asthma & Immunology Research. Published on 2014;6(5):389-400 ,15Azad MD, et al. Impact of material intrapartum antibiotics, method of birth and breastfeeding on gut microbiota during the first year of life: a prospective cohort study. Published on BJOG.2015 ,16Haahtela T, Holgate S, Pawankar R, Akdis CA, Benjaponpitak S, CaraballoL, et al. The biodiversity hypothesis and allergic disease: world allergy organization position statement. World Allergy … Continue reading

As 70-80% of immune cells are located in the gut, the immune system development relies on establishing a balanced and diverse gut microbiota in early life18Vighi G, et al. Allergy and the gastrointestinal system. Clinical and Experimental Immunology, 153 (Suppl. 1): 3–6 ,19West CE et al. J Allergy Clin Immunol. Published on 2015;135:3-13 ; well developed gut microbiota populations are associated with improved health later in life, including reduced risk of allergies and persistence of allergic diseases.20Vighi G, et al. Allergy and the gastrointestinal system. Clinical and Experimental Immunology, 153 (Suppl. 1): 3–6
There are consistent associations between reduced infant intestinal biodiversity and allergic diseases. Infants with cow’s milk allergy or multiple food allergies have been shown to have gut microbiota dysbiosis, which may continue even after allergic symptoms have resolved.24Penders J, Gerhold K, Stobberingh EE, et al. Establishment of the intestinal microbiota and its role for atopic dermatitis in early childhood. J Allergy Clin Immunol.Published on 2013;132:601-607.e8 ,25Bisgaard H, Li N, Bonnelykke K, et al. Reduced diversity of the intestinal microbiota during infancy is associated with increased risk of allergic disease at school age. J Allergy Clin Immunol, … Continue reading,26Storro O, Avershina E, Rudi K. Diversity of intestinal microbiota in infancy and the risk of allergic disease in childhood. Curr Opin Allergy Clin Immunol. Published on 2013;13:257-62 ,27Bisgaard H, Bonnelykke K, Stokholm J. Immune-mediated diseases and microbial exposure in early life. Clin Exp Allergy. Published on 2014;44:475-81
Exposure to antigens early in life
Antigens, including allergens, are substances that enter the body and trigger an immune response. The immune system needs to learn to recognise which substances are beneficial, such as foods, and which are harmful, such as certain bacteria. Based on this identification and assessment, the immune system develops a mechanism that allows it to tolerate certain antigens or clear other antigens. The first time the body encounters a new antigen, it will take days before the immune response is complete.

Tolerating the nutritional components of food is an active response by the immune system.
As the immune system has now learned that this substance could be harmful, it will be much quicker to respond when next exposed to the same antigen. This is the basis of our adaptive immune function. Reduced exposure to antigens in early life, and therefore a failure to educate the immune system appropriately, is another major contributing factor to the rise in allergy.28Azad MD, et al. Impact of material intrapartum antibiotics, method of birth and breastfeeding on gut microbiota during the first year of life: a prospective cohort study. Published on BJOG.2015 ,29Brooks et al, Published on 2013 ,30Kramer et al, 2013 and Azad, Published on 2015 /
Conversely, early exposure to antigens (including those arising from a diverse microbiota) is central to the development of a trained immune system, which in turn is an important factor in the prevention of allergies.
View References
| 1 | Prescott, S.L, Origins: Early-life solutions to the modern health crisis, Published on 2015: University of Western Australia Press, Crawly, Western Australia. |
|---|---|
| 2, 9, 10, 12, 13 | Prescott SL, J Allergy Clin Immunol. Published on 2013;131(1):23-30 |
| 3, 11 | Pawankar R, et al. World Allergy Organisation (WAO): White book on allergy. Wisconsin: World Allergy Organisation. Published on 2011 |
| 4 | Fiocchi A, et al. World Allergy Organization Journal. Published on 2010;3(4):57-161 |
| 5 | Gupta R, JAMA Pediatrics. Published on 2013;167:1026-31 |
| 6 | Patel DA J Allergy Clin Immunol. Published on 2011;128:110-5 |
| 7 | Sladkevicius E and Guest JF, J Med Econom. Published on 2010;13:273-83 |
| 8 | Boyle Allergy, Published on 2016;71:701-710 |
| 14 | Kim BJ et al. Environmental changes, microbiota and allergic diseases. Allergy, Asthma & Immunology Research. Published on 2014;6(5):389-400 |
| 15, 28 | Azad MD, et al. Impact of material intrapartum antibiotics, method of birth and breastfeeding on gut microbiota during the first year of life: a prospective cohort study. Published on BJOG.2015 |
| 16 | Haahtela T, Holgate S, Pawankar R, Akdis CA, Benjaponpitak S, CaraballoL, et al. The biodiversity hypothesis and allergic disease: world allergy organization position statement. World Allergy Organization Journal. Published on 2013;6(1):3 |
| 17 | Weizman Z. Dysbiosis – the concept of dysfunctional intestinal microbiota. In: Intestinal Microbiota Probiotics and Prebiotics: Comprehensive Textbook for Health Professionals, R. Orel (ed); Ljubljana Institute for Probiotics and Functional Foods. Published on 2014 |
| 18, 20, 21 | Vighi G, et al. Allergy and the gastrointestinal system. Clinical and Experimental Immunology, 153 (Suppl. 1): 3–6 |
| 19, 22 | West CE et al. J Allergy Clin Immunol. Published on 2015;135:3-13 |
| 23 | Mitsuoka T. Nutr Rev. Published on 1992;50:438-446 |
| 24 | Penders J, Gerhold K, Stobberingh EE, et al. Establishment of the intestinal microbiota and its role for atopic dermatitis in early childhood. J Allergy Clin Immunol.Published on 2013;132:601-607.e8 |
| 25 | Bisgaard H, Li N, Bonnelykke K, et al. Reduced diversity of the intestinal microbiota during infancy is associated with increased risk of allergic disease at school age. J Allergy Clin Immunol, Published on 2011;128:646-52.e1-5 |
| 26 | Storro O, Avershina E, Rudi K. Diversity of intestinal microbiota in infancy and the risk of allergic disease in childhood. Curr Opin Allergy Clin Immunol. Published on 2013;13:257-62 |
| 27 | Bisgaard H, Bonnelykke K, Stokholm J. Immune-mediated diseases and microbial exposure in early life. Clin Exp Allergy. Published on 2014;44:475-81 |
| 29 | Brooks et al, Published on 2013 |
| 30 | Kramer et al, 2013 and Azad, Published on 2015 / |